Wider context
- Half of all mental health conditions become established before age 14, and 75% by age 24 (Kessler et al., 2005).
- There has been a substantial rise in the number of children and young people in England who have diagnosable mental health conditions. In 2017, 1 in 9 children aged between 5 and 16 had a probable mental health condition; but 2021, this had risen to 1 in 6 (NHS Digital, n.d.) (note that this survey did not give a full assessment of mental health, and instead estimated the likelihood that a child or young person had a mental health condition, classifying this as either: unlikely, possible or probable).
- Rates of mental health illness are higher than before the COVID-19 pandemic (NHS Digital, 2022), with one estimate suggesting that 5 million children and young people (under 18s) in England will need new or additional mental health support as a direct result of the pandemic (O’Shea, 2020).
- Disruptions to everyday life and the support systems children and young people rely on (including at home and at school) during the pandemic worsened the mental health of some children and young people, which could impact them in later life (Samji et al., 2022a).
- The impact of the pandemic on children’s and young people’s mental health has not been the same for everyone and is likely to exacerbate existing inequalities in mental health (Newlove-Delgado et al., 2022).
- The cost of living crisis is impacting thousands of families, with many young people feeling the impact of financial stresses (Mental Health Foundation, 2023). A national survey of parents and carers carried out in 2022 found that 85% were concerned about how the cost of living crisis will affect their families in the next year (The Children’s Society, 2022).
- Even before the COVID-19 pandemic and the cost of living crisis, specialist mental health services for children and young people were not keeping up with increasing demand, leading to growing waiting lists (Royal College of Psychiatrists, 2021b).
Children and young people (aged 0 – 24) made up 29.5% of the population of Cambridgeshire and Peterborough in 2021 (Office for National Statistics, 2022b). There are almost 4,000 more children and young people in in our local area with a mental health condition in 2022 compared to 2021. It is also important to note that co-morbidity (multiple mental health conditions) is relatively common. For example, depression and anxiety often co-occur in young people (Cummings et al., 2014).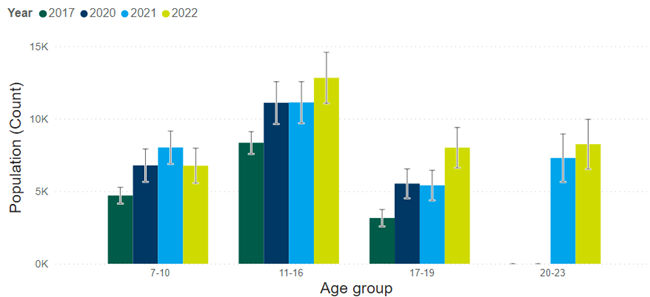
Figure 3: Estimated number of children and young people in Cambridgeshire and Peterborough with a ‘probable’ mental health condition. Data source: dashboard. Note that estimates for young people aged 20 to 23 are not included for 2017 and 2020, as national data did not include this age group. This survey did not give a full assessment of mental health, and instead estimated the likelihood that a child or young person had a mental health condition, classifying this as either: unlikely, possible or probable.
Why do increasing numbers of children and young people have a mental health condition?
- The reasons behind the rise of mental illness in children and young people are likely to be complex. Some factors that may be contributed include increases in poverty among children and young people, greater pressures on families and family dysfunction, and pressures on young people such as an increasing exam-oriented school system (Parish et al., 2020).
- On top of this, demand for mental health services is rising more quickly than the actual prevalence of mental health conditions. This may be due to greater awareness and openness around mental health, greater levels of lower-level mental health need which do not meet criteria for a diagnosable mental health condition, and the reduced capacity of universal services to support mental health needs after a prolonged period of austerity (Parish et al., 2020).
- There is also the impact of the COVID-19 pandemic. A review of global research identifying many reports of increased depression, anxiety and psychological distress in children and young people over time since the start of the pandemic (Kauhanen et al., 2023).
What is the age of onset of mental illness?
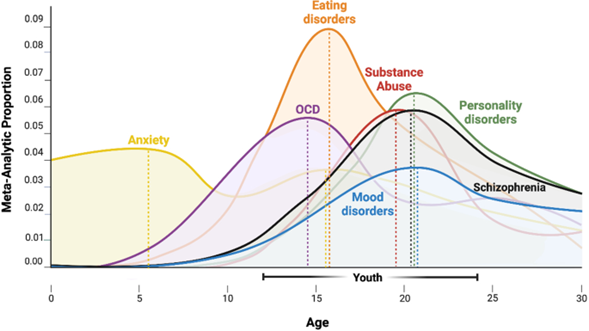
A meta-analysis of studies on this subject found that the median age of onset of mental health conditions is 18 years (with the interquartile range between age 11 and 34) (Solmi et al., 2022). This highlights the importance of identifying risk and mitigating mental health problems in children and young people; as well as ensuring that mental health services are accessible at this crucial age range.
Figure 2: Age of onset of mental disorders. Image source: Towards a youth mental health paradigm: a perspective and roadmap
The age of onset varies by condition. This meta-analysis found that there was generally little difference between studies that defined ‘onset’ by first symptoms, first diagnosis or first hospitalisation; other than symptoms presenting many years before first diagnosis for substance use/addictive behaviours (median 9 years earlier) and mood disorders (median 8 years earlier).
How can local partners work together effectively to support mental health and wellbeing?
A report commissioned by the Local Government Association in 2019 identified three ways of working and nine key enablers to improving children and young people’s mental health and emotional wellbeing (Parish et al., 2020). These are summarised below (Parish et al., 2020):
- Making children and young people’s mental health and wellbeing a shared priority
- Leadership and vision: political leaders who advocate for children and young people’s mental health; and senior officers and leaders promoting partnership working across the system.
- Self-reflective partnership: robust governance structures with a clear agreement of what partnerships aim to achieve. Partnerships should be built on trusting relationships.
- Integrated commissioning: shared commissioning plans and objectives between local authorities and the ICS, to create a good environment for spending decisions.
- Focusing on and investing in earlier intervention and prevention
- Working with young people: meaningful inclusion of young people at each level of the system, from service feedback to shaping system priorities.
- Promoting good mental health: working with universal services, such as perinatal services, schools and youth centres, was thought to be key for prevention and earlier intervention.
- Developing the children’s workforce: equipping professionals who work with children, such as staff in nurseries, schools and youth services, with the skills and knowledge to have supportive conversations about mental health with children and young people.
- Delivering specialist support differently
- Embedded child and adolescent mental health services (CAMHS): integrating specialist mental health expertise in the delivery of key services supporting children and young people.
- Supporting families: holistic family-based support, such as around parental conflict and parental mental health conditions.
- Creative solutions to managing risk: exploring how best to support children and young people with complex mental health or emotional challenges, whose needs may not always be met by traditional approaches offered by CAMHS.
Figure 4: Themes for establishing an effective partnership-based approach to supporting children and young people’s mental health. Image source: Building resilience: how local partnerships are supporting children and young people’s mental health and emotional wellbeing
Additional resources
- State of the nation 2022: children and young people’s wellbeing
- Children and young people’s mental health: An independent review into policy success and challenges over the last decade
- Building resilience: how local partnerships are supporting children and young people’s mental health and emotional wellbeing
References
Full list of references is included at the end of this chapter.