Inpatient
- Acute inpatient services provide treatment when a person’s mental health condition cannot be managed in the community, and where specialist care is required in a safe and therapeutic setting (Public Health England, 2019). Inpatient admissions should be purposeful, integrated with other services, open and transparent, and as local and short as possible (Care Quality Commission, 2015).
- Although mental healthcare is often discussed in terms of inpatient treatment, only around 3% of people accessing mental health services in 2018/19 received inpatient care (Davidson, 2021).
- Nationally, inpatient mental health services are managing increasing demand and acuity, alongside the wider workforce pressures across the NHS (NHS England, 2023b).
- The GIRFT view is that NHS mental health provision should be thought of as a community-based secondary care service, to which an acute inpatient service is attached to serve people when access is essential. Community mental health services play a crucial role in delivering mental health care for adults and older adults with severe mental health needs as quickly and as close to home as possible. Inpatient care, when it is essential, should also be accessible locally and rapidly (Davidson, 2021).
Data from Cambridgeshire and Peterborough suggests there are both strengths and areas for improvement in local inpatient services. The vast majority of people admitted to hospital are already known to community mental health services, and the number of admissions where people are detained under the Mental Health Act are decreasing. However, there are high levels of occupancy of acute mental health beds and an increasing number of inappropriate out of area placements compared to previous years. More people are spending over 60 days in inpatient care. Contributing factors to this may include:
- Staffing pressures, which led to the closure of Mulberry Ward 3.
- Increase in mental distress (demand and acuity), due to the cost of living crisis and wider impacts of the COVID-19 pandemic
- Greater acuity when people become inpatients because of delays to admission (finding beds)
- Greater reliance on out of area placements, which are associated with greater length of stay
- Delays to discharge because of wider system pressures (such as in housing and social care)
Pathways into inpatient care
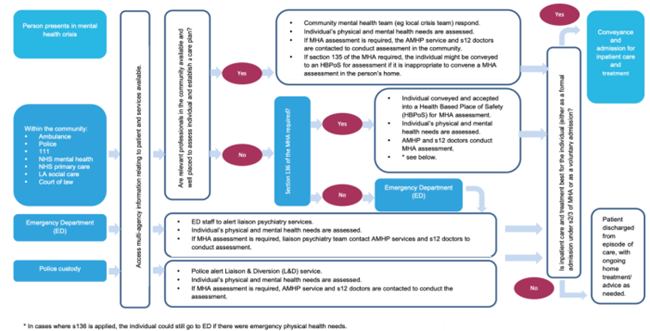
There are a range of pathways into inpatient care for people experiencing mental health crisis. The diagram below reflects key pathways in our local system, although it does not capture all routes into inpatient care such as the joint mental health response car, or alternatives to inpatient care such as The Sanctuary.
Figure 58: Pathways from mental health crisis into inpatient care. Image source: Access to mental health inpatient services in London (all ages)
Wider context
National context
The Strategy Unit’s 2019 report Exploring Mental Health Inpatient Capacity across Sustainability and Transformation Partnerships in England summarised the increasing demand on inpatient mental health services across England:
- Since the 1970s/80s, mental health services have shifted away from focusing on inpatient services to community-based care. From 1989 to 2019, there was a 73% reduction in the number of mental health beds across England. This reduction has been managed by a reduction in the number of people admitted to hospital and a reduction in the length of time people spend in hospital.
- National data shows that from the mid-2000s, the length of time people spent as inpatients has not decreased. The level of mental ill health of people admitted to hospital in 2018 was greater than that in 2013, which may indicate that thresholds to accessing an inpatient bed have increased over recent years.
- People with lived experience report not being able to access inpatient care when they need it. Healthcare professionals report that wider system pressures have contributed to challenges around inpatient beds, including staff shortages, pressures on community mental health services and social and demographic changes.
National policy
- The Crisp Review (2016) highlighted pressures on mental health beds and recommended an end to acute out of areas admissions (Commission to review the provision of acute inpatient psychiatric care for adults, 2016). The Government adopted this goal, with the aim to end inappropriate out of area placements by 2020/21. However, this target has not been met across England.
- The Royal College of Psychiatrists state that ‘challenges to reduce the persistently high rates of inappropriate out of area placements and provide timely access to and discharge from acute inpatient services remain substantial’, due to a lack of capacity in the system to meet the population level of mental health need (Royal College of Psychiatrists, 2019b).
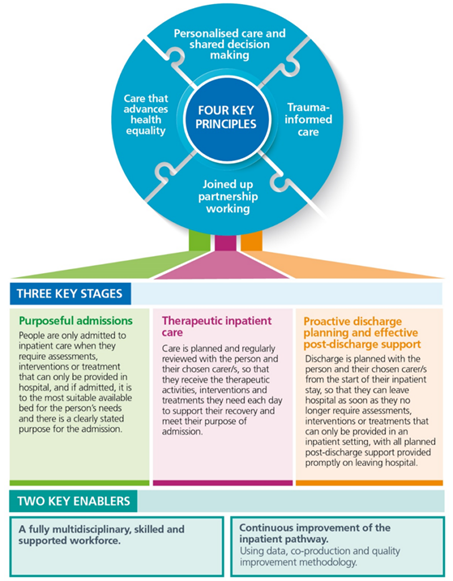
- In 2023, NHS England produced a national policy document supporting the commissioning of acute inpatient mental healthcare for adults and older adults. This identified key elements of effective inpatient mental healthcare, with four key principles, three key stages and two key enablers.
Figure 59: Key elements of the inpatient pathway. Image source: NHS England
Local context
- In Cambridgeshire and Peterborough, acute mental healthcare is based on the ‘333 model’, where inpatient pathways for assessment are provided within 3 days, treatment within 3 weeks and recovery within 3 months (Ray et al., 2019).
- This model is focused on recovery, and aims to improve access to healthcare, delivery early treatment and reduce the length of hospital stays.
- There are three pathways through inpatient care, for which the typical length of stay varies:
- Assessment unit – 3 days (Mulberry 1): provides a safe holding environment for patients and enables a thorough assessment of mental and physical health needs, and social circumstances.
- Interventions unit – 3 weeks (Mulberry 2): patient’s needs and strengths are assessed, and collaborative care plans are developed. This may include a social as well as pharmacological and psychological interventions.
- Recovery unity – 3 months (Mulberry 3): takes a recovery-based approach to meet the needs of patients with more complex needs. This includes intensive support from staff, to meet long-term recovery goals. This ward was closed in May 2022.
- The community mental health team and crisis home resolution treatment team (CRHTT) supports the 333 model in the community, including by setting expectations of admission.
Minimising restrictive practises is a national priority (Department of Health and Social Care, 2018). CPFT has previously been a national leader in this endeavour. PROMISE (PROactive Management of Integrated Services and Environments) was developed by CPFT staff and people with lived experience to reduce coercive practises and use of force. Over a 3-year period, CPFT experienced a dramatic reduction in all forms of restraint as well as registering high patient experience scores. This was achieved through a transformation of ward culture using PROMISE’s five-step governance framework (Report, Reflect, Review, Rethink and Refresh). Unfortunately, the benefits lessened in the context of the COVID-19 pandemic. However, it is proposed that this programme be re-activated in a refreshed form.
What do people say?
National reports highlight that:
- Some people who access inpatient care report positive experiences, whilst others experience issues in accessing care that meets their needs. This can include delays in accessing inpatient services and disproportionate use of restrictive practices (NHS England, 2023b).
- Being placed out of area can be particularly difficult for individuals and their family, friends or carers, due to the distance from support networks and disruption in continuity of care (NHS England, 2023b).
- Culture is key for both patients and staff. Patients need a ‘kind, compassionate and hopeful’ experience to feel safe and make progress; and staff also need to feel safe and supported to speak up when services to not meet the standards they want to provide (Department of Health and Social Care, 2023).
- Pathways for giving feedback are not always clear or easy to use for patients, carers or staff. Despite this, many staff report feeling frustrated at the amount of time they spend inputting data into different systems, which can take away from time they spend with patients (Department of Health and Social Care, 2023).
As part of the Cambridgeshire and Peterborough Mental Health Act Assessment Pathway Review (2023), people with lived experience of the pathway (including as carers) highlighted the following issues relating to high levels of occupancy in local inpatient services:
- Delays in informal admissions when a person would have previously been admitted as an inpatient. As a result of this, people are supported in the community, which can have a detrimental impact on their mental state, as well as cause distress and anxiety to carers.
- Community mental health teams are already under significant pressure due to staff vacancy rates and managing existing demand and are having to prioritise people with the greatest level of need, potentially leading to more people relapsing and needing inpatient admission or a Mental Health Act assessment.
- Planned Mental Health Act assessments are not completed when an identified bed is not available.
- Inappropriate out of area placements (OAPs) have a detrimental impact upon the individual’s recovery and means that they can be placed hundreds of miles away from their family and support network.
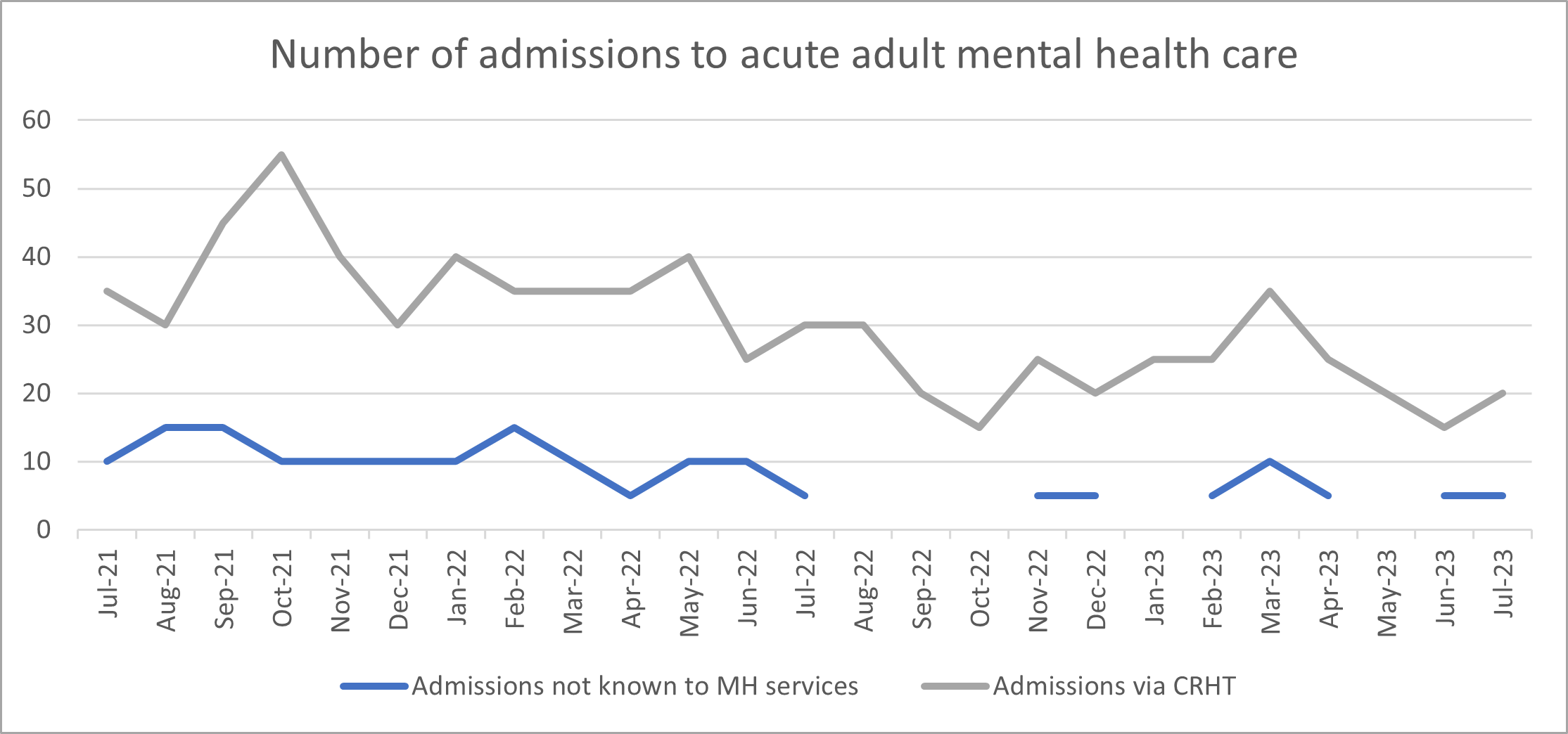
Admissions
In Cambridgeshire and Peterborough ICS, the number of admissions to adult acute inpatient mental health care via the crisis resolution team shows a declining trend. The number of adult acute mental health admissions and the percentage of admissions with no previous contact show no significant change between February 2022 and July 2023.
Figure 60: Admissions to adult acute inpatient mental health care, Cambridgeshire and Peterborough ICS, July 2021 – July 2023. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
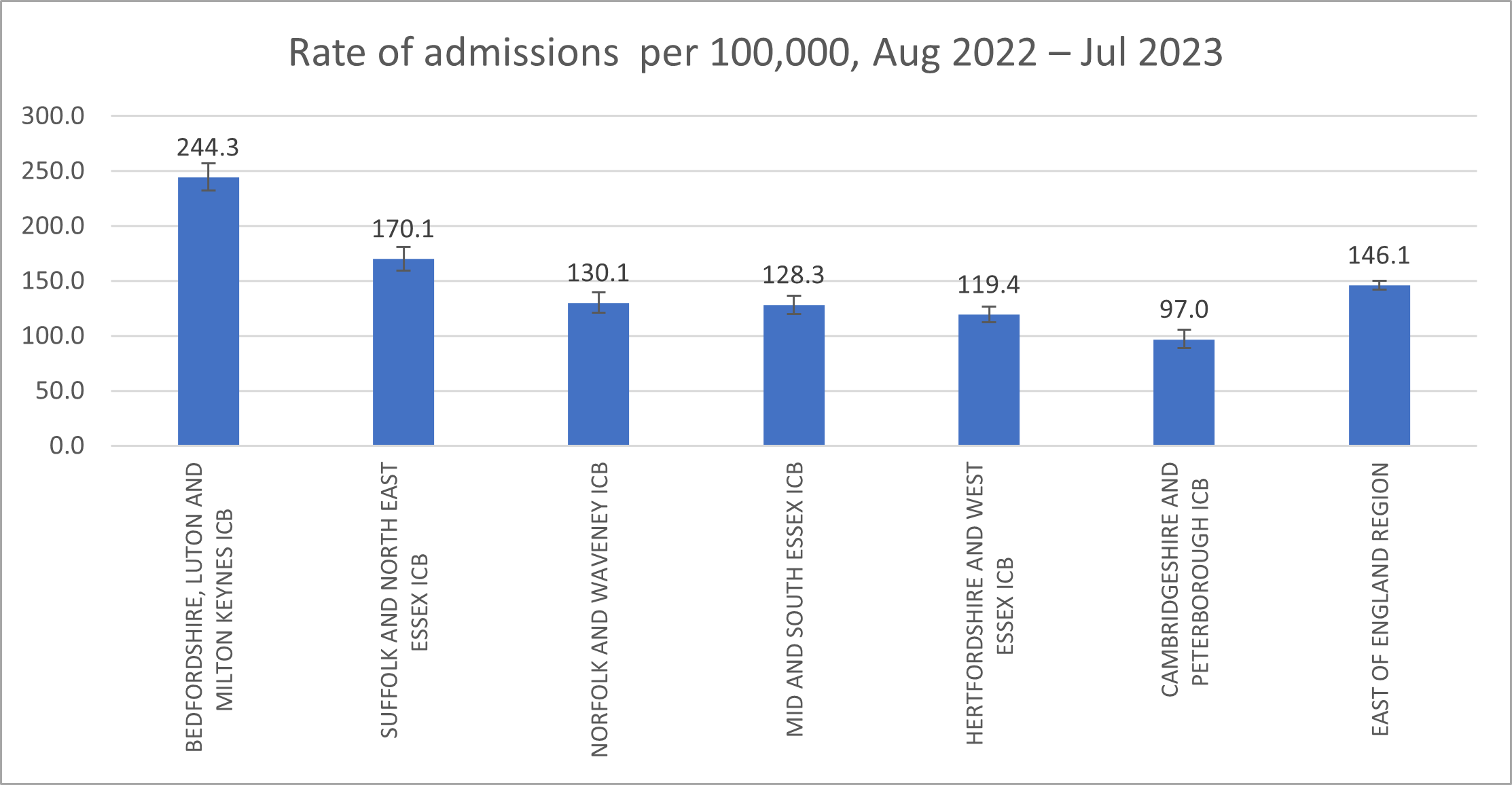
In August 2022 to July 2023, the rate of admissions to acute inpatient mental healthcare per 100,000 of the population was significantly lower in Cambridgeshire and Peterborough compared to other areas in the East of England.
Figure 61: Rate of admissions to adult acute inpatient mental health care per 100,000 of the general population, East of England, August 2022 – July 2023. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
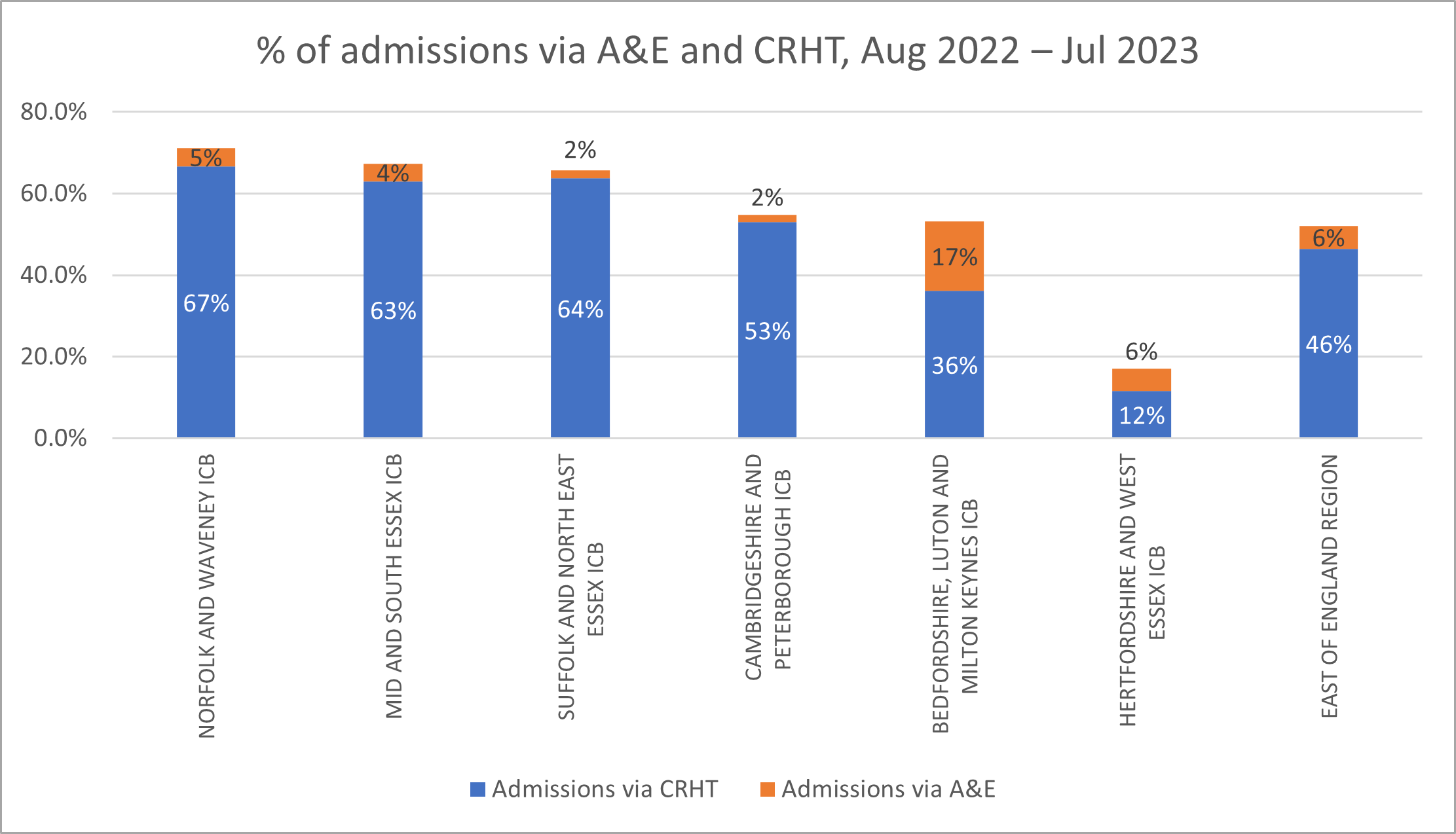
 53% of admissions to acute adult inpatient care in Cambridgeshire and Peterborough ICB were admitted through the Mental Health Crisis Resolution Home Team (CRHT), and 2% through Accident and Emergency
53% of admissions to acute adult inpatient care in Cambridgeshire and Peterborough ICB were admitted through the Mental Health Crisis Resolution Home Team (CRHT), and 2% through Accident and Emergency
Figure 62: Route of admissions to adult acute inpatient mental health care, East of England, August 2022 – July 2023. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
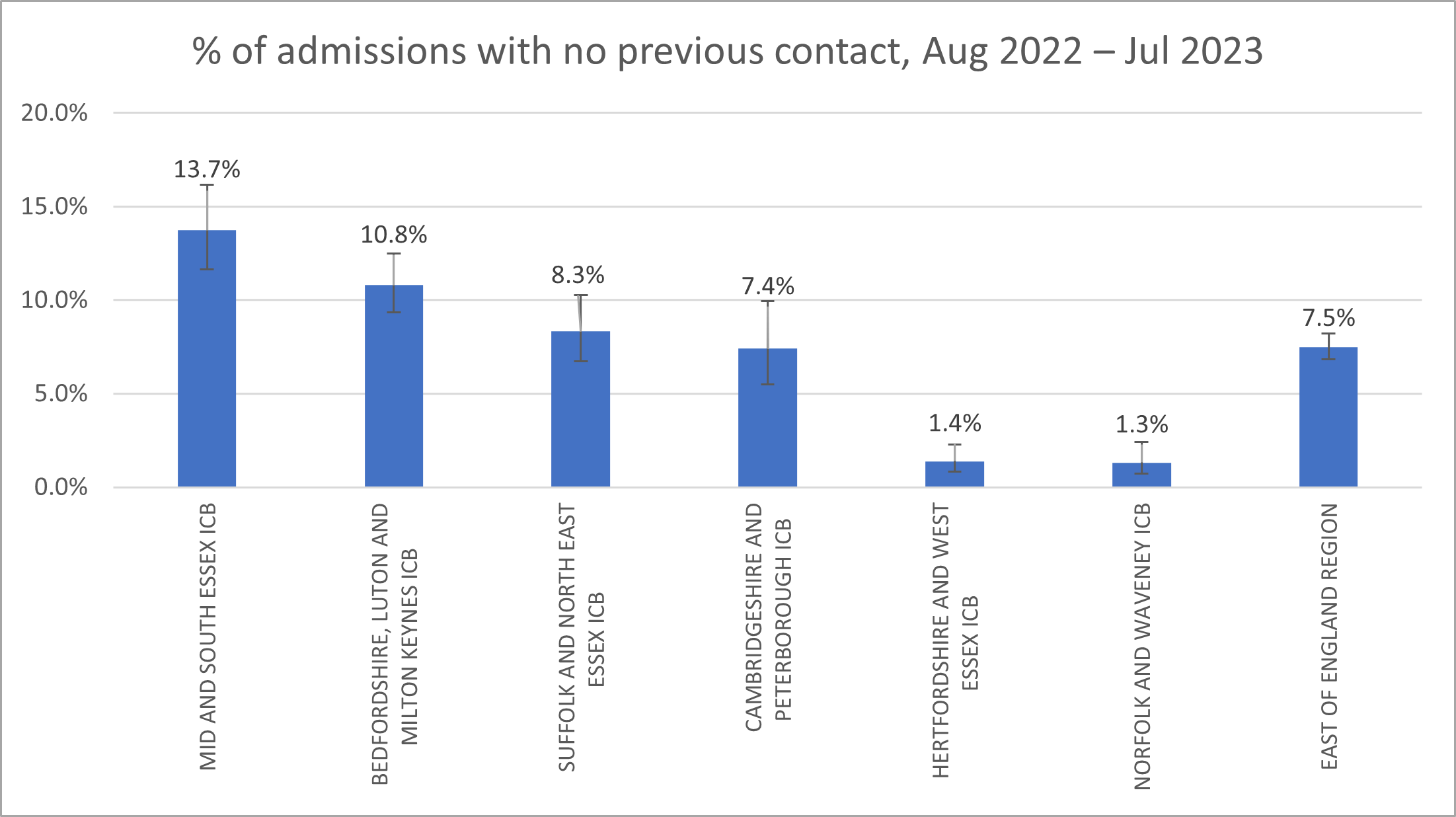
7.4% of people to admitted to inpatient care from August 2022 to July 2023 had not been in contact with core community mental health services within the period 6 months prior to admission, which is statistically similar to the East of England average. This group may include some people who were in contact with other services to support their mental health (such as voluntary sector organisations or primary care).
Figure 63: Proportion of admissions to adult acute inpatient mental health care with no contact with core mental health services in the past 6 months, East of England, August 2022 – July 2023. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
National research suggests that a quarter (26%) of cases where people are admitted to acute hospital for any reason, there have been missed opportunities to make interventions that would be prevented the need for admission (Local Government Association, 2016). There are no statistics which are specific to admissions to acute mental healthcare or our local area.
How many people are admitted under the Mental Health Act?
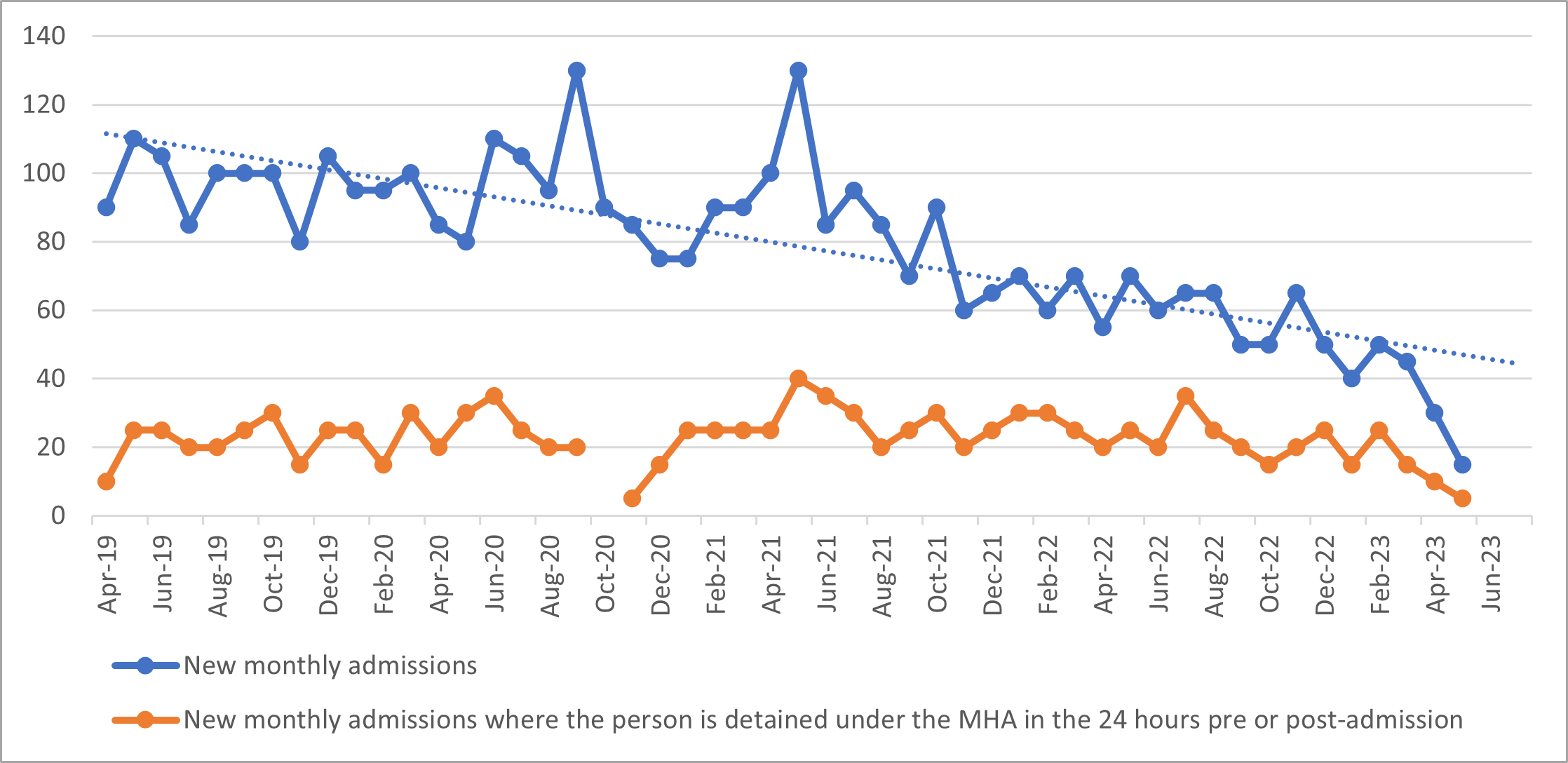
The number of new monthly inpatient admissions has substantially decreased over the last couple of years in Cambridgeshire and Peterborough. A shortage of beds may have contributed to this trend. The number of new monthly admissions where the person is detained under the MHA in the 24 hours pre-admissions or post-admissions shows a relatively stable trend.
Figure 64: New monthly admissions and new monthly admissions where the person is detained under the MHA in the 24 hrs pre- or post-admission, Cambridgeshire and Peterborough ICS, April 2019 – June 2023. Data source: MHA Dashboard – Mental Health, Learning Disability and Autism Resource Hub – FutureNHS Collaboration Platform
How many people are admitted into detox beds?
- NICE guidelines highlight that people in acute alcohol withdrawal, or those who are high risk, should be offered admission to hospital for medically assisted alcohol withdrawal (‘detoxification’ or ‘detox’) (National Clinical Guidelines Centre, 2010).
- There were previously 3 inpatient detox beds in Cambridgeshire, based in the Mulberry 1 Ward (CPFT). Since the Cambridgeshire drug and alcohol treatment system was recommissioned in October 2018, inpatient beds have been purchased by Change Grow Live (CGL) from a range of providers across the county. Regionally commissioned inpatient beds are now based in Chelmsford.
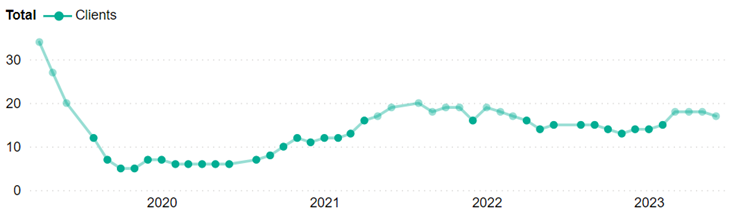
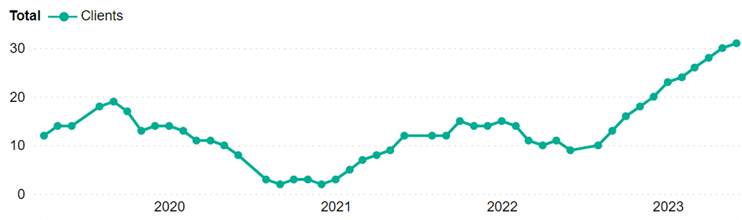
In June 2023, there were 17 inpatients in detox beds in June 2023 in Cambridgeshire, and 17 in Peterborough. The trends in inpatient uptake of detox beds may reflect the availability of beds: there was a decrease in inpatient uptake in Cambridgeshire from 2019, when the number of beds declined; whist the increase in uptake in Peterborough from 2023 may have been due to greater investment in provision through the Drugs Strategy.
Figure 65: Inpatient uptake of detox beds, Cambridgeshire, July 2022 to June 2023. Data source:
Figure 66: Inpatient uptake of detox beds, Peterborough, July 2022 to June 2023. Data source:
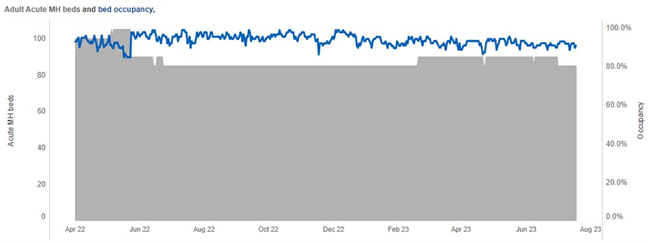
How many beds are occupied?
- High levels of bed occupancy are an important measure of pressure on the acute mental health pathway. For patients, this can mean that they are not admitted to hospital until they are very unwell (Liberati et al., 2023).
- The Royal College of Psychiatry suggests that 85% is the maximum level of occupancy of mental health beds (Royal College of Psychiatrists, 2019c). Spare bed capacity is important to manage variation in demand and make sure that patients can flow smoothly through the system.
- From 2010/11 to Q3 2022/23, there was a 23% decrease in the number of mental health beds in England, from 23,515 to 18,152 beds (Nuffield Trust, 2023).
- In June 2023, 75 out of 85 (91%) of adult acute mental health beds in Cambridgeshire and Peterborough NHS Foundation Trust (CPFT) were occupied.
- The Mulberry 3 Ward, a 16-bed treatment ward (13 acute and 3 forensic step-down beds), was closed on 21st May 2022 due to staffing pressures. This is likely to have contributed to pressures on bed occupancy and there are plans to reopen this ward when enough staff have been recruited.
Figure 67: Adult acute mental health beds (grey) and occupancy (blue) in Cambridgeshire and Peterborough ICS, April 2022 – June 2023. Data source: Workbook: Adult acute mental health benchmarking dashboard (england.nhs.uk)
Research suggests that there should be between 30 to 60 psychiatric beds per 100,000 of the population (Mundt et al., 2022).
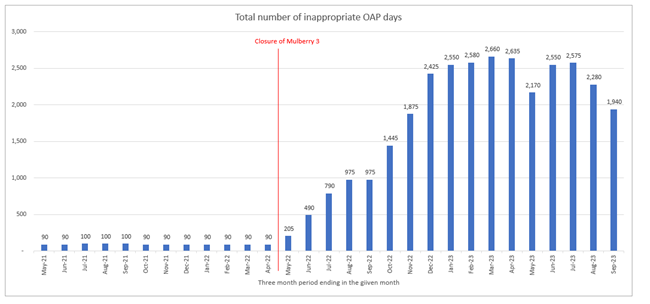
Out of area placements
Inappropriate placement of mental health patients in hospitals outside their local area (known as inappropriate out of areas placements or OAPs) occur when suitable inpatient provision is not available locally. Appropriate out of area placements are made when a specialist service is not provided locally.
- Inappropriate out of area placements reflect pressures on mental health services and staff (Department of Health & Social Care, 2023), often from a combination of high admission rates, long hospital stays and delays in discharge (NHS England, 2023b).
- Service users report that out of area placements can be hugely detrimental, as they are isolated from local support networks and local services that they may have previously been supported by. This places immense pressures on families and loved ones, for whom it may be unaffordable to travel long distances; and can make it harder for staff to plan and coordinate post-discharge care.
- The number of out of area placements from patients within Cambridgeshire and Peterborough ICS has risen substantially since April 2022. Before this time, the days spent in out of area placements was between 90 to 100 in each three-month period, compared to 2660 in the period ending in April. This represents an over 20 times increase in out of area days from April 2022 to April 2023 (NHS Digital, 2023).
- During the period ending September 2023, there were 1,940 OAP days, and a decline is seen since the period ending July 2023.
- The closure of the Mulberry Ward 3 (which had 16 beds) in May 2022 may account for nearly half out of area bed days in the three months to June 2023. The reduction in out of area placements may be due to recent quality improvement efforts to improve patient flow, including a new patient flow group and dashboard to help with flow (NHS Digital, 2023).
- The average costs of inappropriately out of area placements for Cambridgeshire and Peterborough is £625 per bed each day (interquartile range £600 to £750); with a total of cost of £1,729,589 in April to June 2023. 96% of this cost was due to inappropriate placements (NHS Digital, 2023).
Figure 68: Total number of inappropriate out of area days in Cambridgeshire and Peterborough ICS in the three-month period ending in the given month, May 2021 – September 2023. Data source: Out of Area Placement Report, NHS Futures
Note that bed days are counted as the total number of beds (available or occupied) on each day, as a total sum of all the days in the month (NHS, 2020). For example, if there were 100 beds available over 30 days, there would be 100 x 30 = 3,000 bed days. This is a simplified example as the number of beds often varies daily.
There has been a sustained decline in the number of inappropriate out of area placements since the summer of 2023 and there are plans to reopen Mulberry 3.
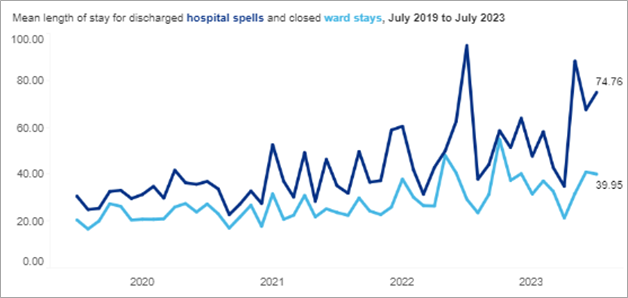
Length of stay
Delays in the transfer of care are a major issue in mental health providers in England (Public Health England, 2019), with the CQC highlighting in 2023 that ‘insufficient capacity in adult social care is continuing to contribute to delays in discharging people’ from hospitals (across the entirety of the healthcare system) (Care Quality Commission, 2021). There is however international research which highlights effective interventions to improve the discharge process (Tyler et al., 2019).
The average length of stay of hospital spells and closed ward stays in Cambridgeshire and Peterborough has increased since July 2019.
Figure 69: Mean length of stay for discharged hospital spells and closed ward stays, Cambridgeshire and Peterborough ICS, July 2019 to July 2023. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
The average length of stay for discharged hospital spells in Cambridgeshire and Peterborough ICB is higher than the regional average.
Figure 70. Mean length of stay for discharged hospital spells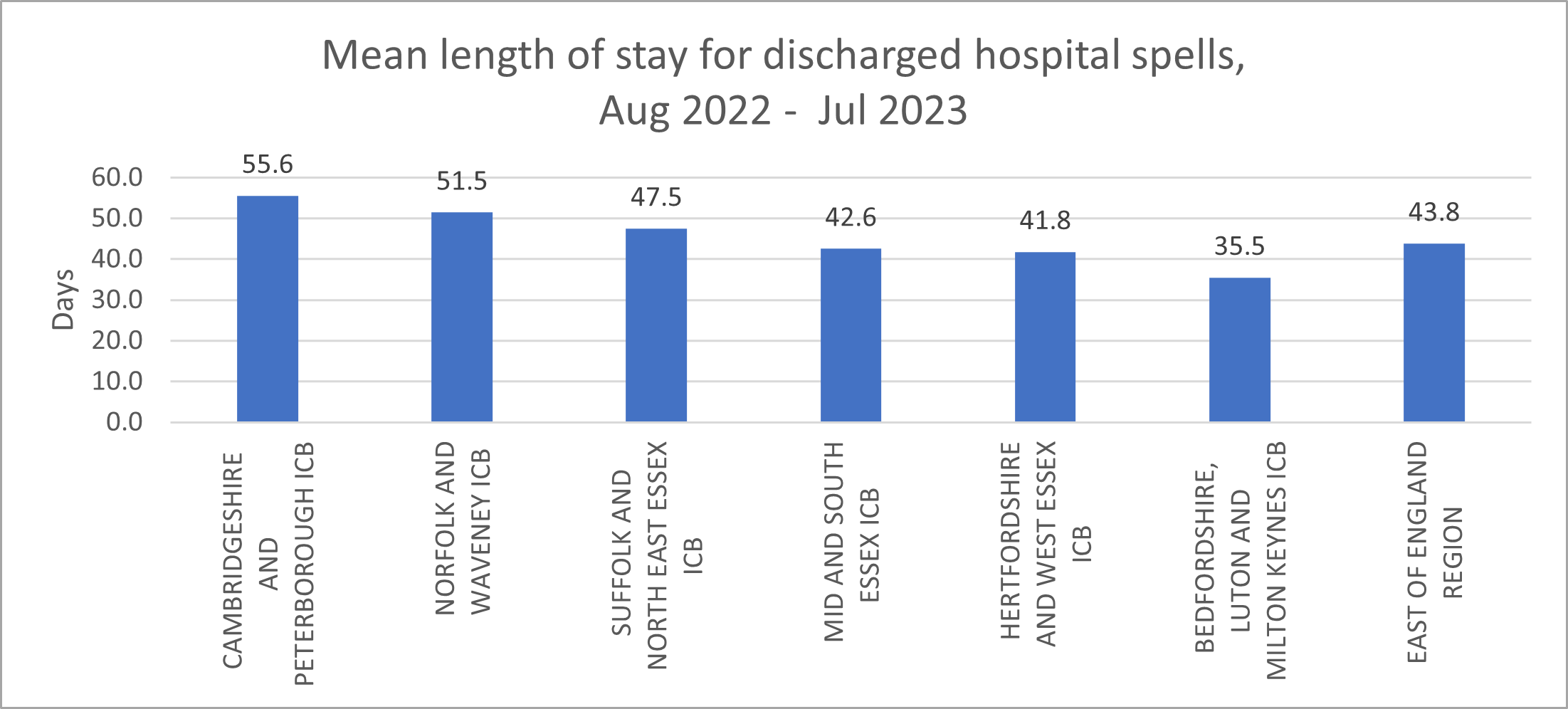
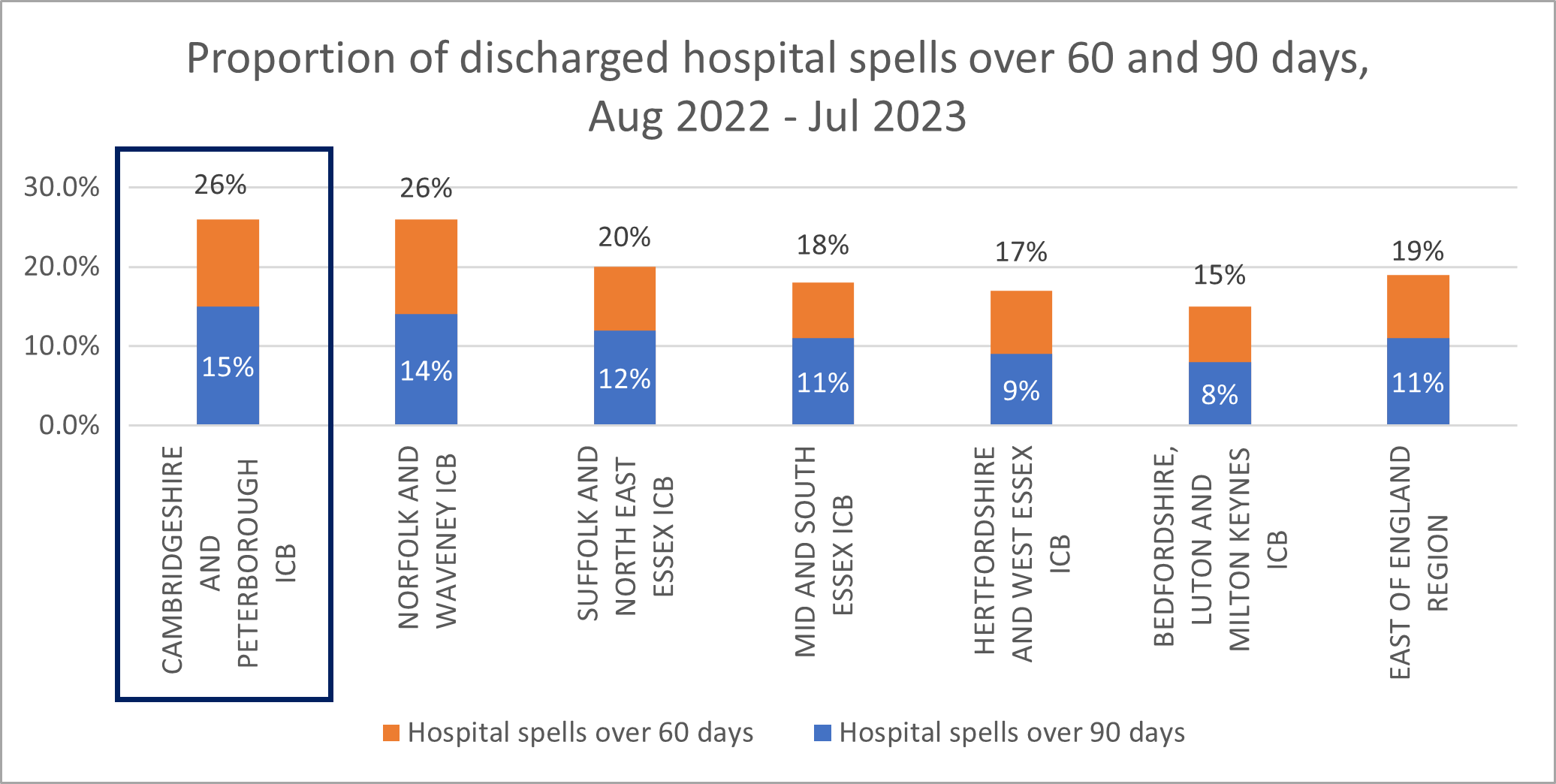
When explored in more detail, there has not been a significant change in the proportion of people spending over 60 days in hospital from February 2022 to July 2023. However, from August 2022 to July 2023, Cambridgeshire and Peterborough ranked highest for the proportion of discharged hospital spells where the length of stay is over 60 days (26%) and 90 days (15%) compared to other areas in the East of England.
Figure 71: Proportion of discharged hospital spells less than 3 days and over 60 days, East of England, August 2022 – July 2023. Source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
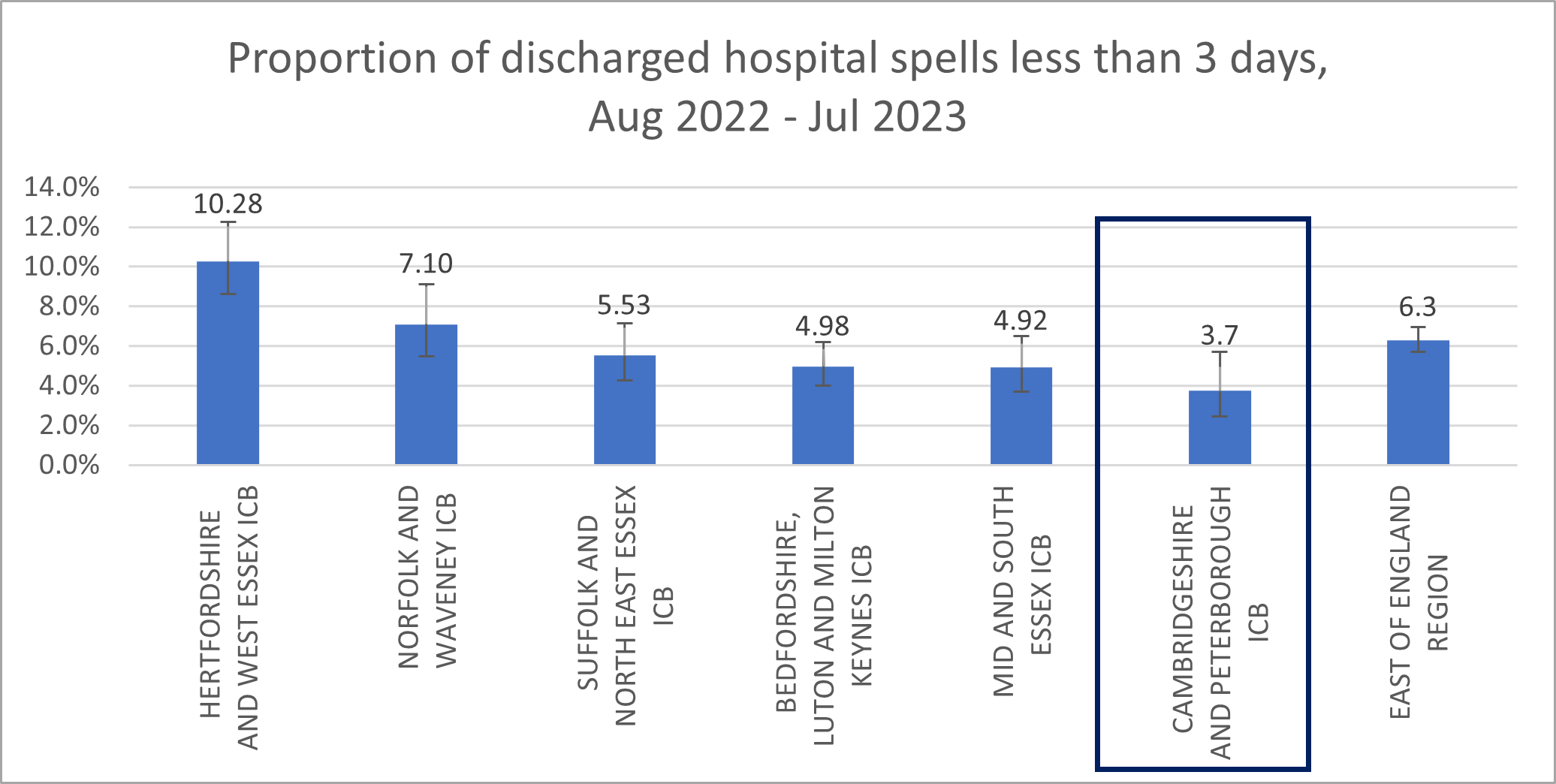
For the period between August 2022 and July 2023, the proportion of discharged hospital spells where the length of stay was less than 3 days was significantly lower in Cambridgeshire and Peterborough ICB compared to the East of England average.
Figure 72: Proportion of discharged hospital spells less than 3 days, East of England, August 2022 – July 2023. Source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
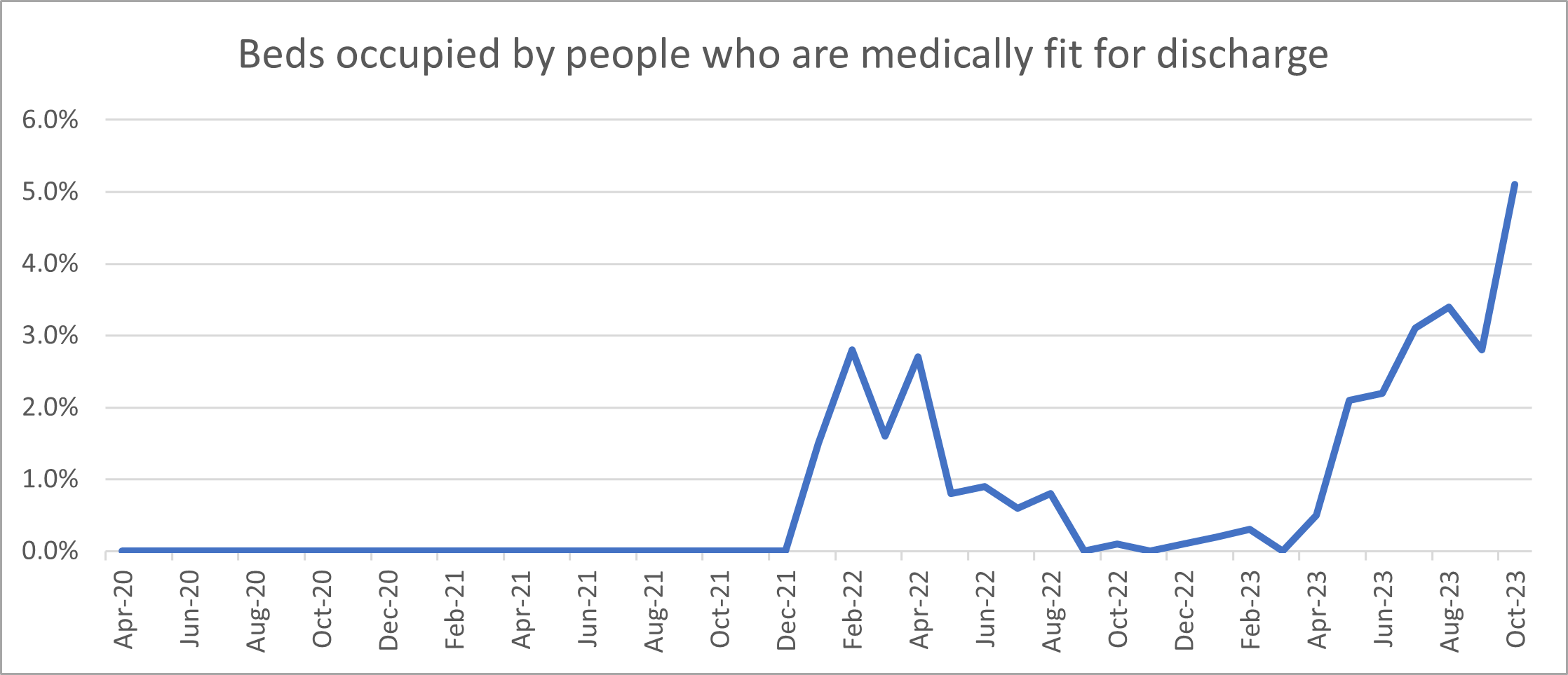
The proportion of beds occupied by people who are medically fit for discharge show an increasing trend since March 2023; though is still relatively small overall
Figure 72: Mental health inpatient bed occupancy by adults (aged 18+) who are clinically ready for discharge, Cambridgeshire and Peterborough ICB, April 2020 – October 2023. Data source: Workbook: All Age UEC Pathway Pressures (england.nhs.uk)
Outcomes
- In 2019/20, an NHS target (CQUIN indicator) was introduced that at least 80% of adults should be followed up within 72 hours of discharge from mental health inpatient care. This target was introduced based on evidence showing that there is an increased risk of dying by suicide 2 to 3 days after being discharged from hospital (Appleby et al., 1997).
- This target has not been met nationally since data became available in June 2020, with 73% of adults receiving a follow up within 72 hours in April 2023 (The Nuffield Trust, 2023).
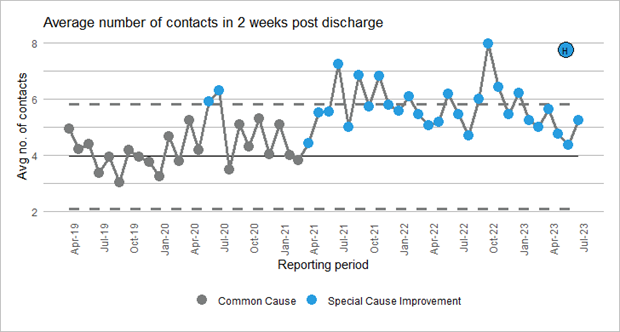
- In Cambridgeshire and Peterborough, the proportion of hospital spells with follow-up within 3 days of the discharge date shows a significant increase since March 2021.
Figure 73: % of adults who were followed up within 72 hours of being discharged from mental health inpatient care. Data source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
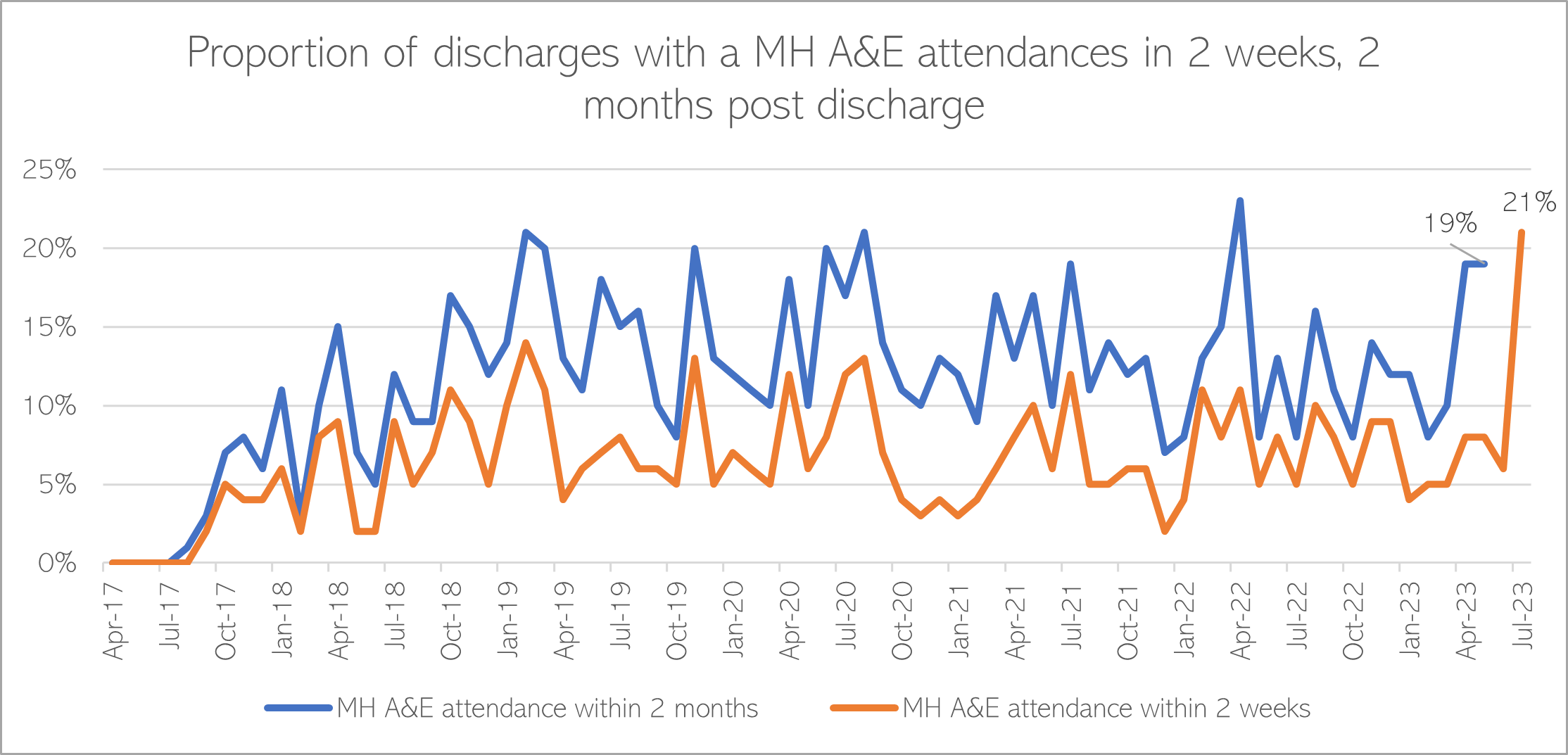
The proportion of people attending Accident and Emergency due to mental health within 2 weeks and 2 months of discharge from hospital shows fluctuations over time.
Figure 74: % of adults had a mental health-related attendance at Accident and Emergency within 2 weeks and 2 months of being discharged from mental health inpatient care. Image source: Workbook: Acute Mental Health Dashboard (england.nhs.uk)
Role of Allied Health Professionals
Art Therapies
Arts Therapies combine creative and psychological processes for therapeutic benefit of patients. They facilitate communication through non-verbal and verbal means and encourage self-expression, rediscovery, renewal, regeneration, and recovery. The arts media used in Arts Therapies can be used to safely explore difficult thoughts and feelings whilst simultaneously facilitating a potential transformative, creative experience in the moment. Arts Therapies signpost patients on to other creative/psychological opportunities after their therapy. In CPFT, Arts Therapies sessions are provided by Arts Therapies clinicians for patients primarily on acute wards and in secondary care. Arts Therapies have clinical spaces in the New Resource Centre Fulbourn and also work across CPFT settings in Huntingdon, Peterborough and Fenland (Wisbech). They are informed by evidence based psychological theory and research.
This includes:
- Art Therapy – facilitates self-expression and exploration. Art can offer an external container for self-expression that can be reflected up on by both the patient and Therapist. Art also offers creativity in the moment which enhances wellbeing. A wide range of Art materials are available.
- Music Therapy – offers a wide range of instruments, pianos, percussion and voice. Music can be improvised, pre-composed or composed.
- Dramatherapy – a wide range of drama and play activities are used including story making, storytelling, working with images, miniatures, games and movement. These are used alongside verbal processing.
Occupational therapy
Occupational therapy provision serves Acute Adult Inpatient Mental Health, Adult Inpatient Learning Disabilities and Psychiatric Intensive Care Unit (PICU) services in the North; and Springbank, George Mackenzie House and Adult Eating Disorder Inpatient services in the South. The clinical purpose of this service is to provide high quality occupational therapy assessment, intervention, and evaluation; supporting people to overcome occupational performance challenges, regain independence, develop functional skills in ADLs and to support mental health recovery through meaningful occupation.
Additionally, their operational purpose is to provide a compassionate, supportive, psychologically safe environment where collaboration, learning, professional development, and service improvement are the shared priorities of our team members. Positive patient outcomes are delivered through collaboratively set patient goals, driven by assessment of strengths, abilities, and areas for skill development across physical, sensory, cognitive, emotional, and social functioning. These assessments guide the direction of occupational therapy intervention which plots measurable goals around the use of meaningful activity, development of daily living skills and establishment of practical coping strategies.
Physiotherapy
The mental health physiotherapy team provides assessment and treatment to adults and older adults in inpatient wards at Fulbourn Hospital and the Cavell Centre, as well as support to people in the adult acute eating disorder unit at Addenbrookes Hospital. Reasons for physiotherapy referrals include orthopaedics, mobility and falls, musculoskeletal, neurology, and to support the inclusion of safe and appropriate physical activity and specialist exercise interventions for improved mental and physical wellbeing. Mental health physiotherapy approaches support patients to engage in treatment and overcome barriers to their physiotherapy treatment that their mental health may present. Physiotherapy input therefore focuses on supporting the individual with their physical health needs, whilst acknowledging their mental health condition, and how mental and physical health are interdependent. The team provide assessment and treatment in the form of individual and groups sessions, both ward-based and within the physiotherapy department, utilising the department-based gym and exercise facilities.
Autism and ADHD
- The National Autistic Society states that ‘it is widely recognised that for most autistic people, care in an inpatient unit is rarely helpful—in fact, it can be deeply damaging’ (NAS, 2023).
- 16% of autistic adults in mental health inpatient settings received a formal autism diagnosis after being admitted into inpatient care (NHS England, 2023d).
- There has been a range of national policies and targets in recent years that have aimed to improve inpatient mental health settings for autistic people, including a renewed focus on reducing admissions of autistic people to inpatient care and increasing discharge rates (NHS England, 2024).
- CPFT is currently part of the national learning disability and autism inpatient quality transformation programme. The programme is built upon the cornerstones of good mental healthcare; continuity of care, therapeutic relationships and a commitment to mental health care meeting the needs of all citizens.
The information below focuses on the experiences and outcomes of autistic people in inpatient mental health settings. Despite the high rate of undiagnosed ADHD in inpatient mental health settings, there is little research into tailored support and treatment for this group (Lines and Sadek, 2018).
Rates of inpatient admissions
- The NHS Long Term set the goal that, by March 2023, the number of autistic people in inpatient mental health settings would fall to half of 2015 levels (NHS, 2019). However, the number of autistic inpatients in England increased from 2015 to 2024 (Abreu, Parkin and Foster, 2024).
- The Care Quality Commission’s report ‘Out of sight – who cares?’ found that autistic people who did not get the care and support they needed in the community, such as due to long waiting lists for an autism assessment or a lack of specialist support services, can end up experiencing a ‘crisis point’ in which the ‘only option’ is mental health inpatient services (CQC, 2020).
- The introduction of the Dynamic Support Register (DSR) and Care (Education) and Treatment Review (C(E)TR) policy aims to prevent unnecessary hospital admissions for autistic people and people with a learning disability (NHS England, 2023b).
Length of stay
National data shows that some autistic people spend long periods of time in inpatient mental health settings. In October 2023, half of people with a learning disability and/or autism in hospitals in England had been in hospital for over 2 years (Tudor, 2023).
Experience
The Care Quality Commission’s report ‘Out of sight – who cares?’ highlights that spending time on noisy and chaotic hospital wards can heighten autistic people’s distress. Some autistic people may express this distress in ways that other people find challenging; and in some cases this behaviour can be ‘managed’ through restraint, seclusion and segregation, rather than by addressing the underlying cause (CQC, 2020). National research involving people with learning disabilities and autistic people (including autistic people with learning disabilities) in long-stay hospital settings, as well as family members, commissioners and healthcare professionals, found that (Glasby et al., 2024):
- People in hospital often feel frustrated and that hospital environments are not environment that is conducive to them getting better or staying well, and that they face multiple barriers to leaving hospital.
- Frontline staff feel they are working a complex system that is extremely difficult to navigate.
- There is not a shared sense of how many people need to be in hospital or could be cared for in different settings across hospital staff.
Additional resources
- The local data packs give an overview of prevalence and service use
- Acute inpatient mental health care for adults and older adults
- Old problems, new solutions: Improving acute psychiatric care for adults in England
- Eliminating Inappropriate Out of Area Placements in Mental Health
- Service Capacity in England from RCPsych
References
Full list of references is included at the end of this chapter.