Eating disorder services
- Young adulthood is the most common age of onset for eating disorders (Treasure et al., 2020). Many people with eating disorders also have another mental health condition (including mood and anxiety disorders) and/or neurodevelopmental conditions (Treasure et al., 2020).
- Nationally, there has been a rise in the number of children and young people presenting to eating disorder services since 2021 (Children’s Commissioner, 2023c).
- In the Children and Young People’s Mental Health Strategy (2022), local stakeholders (mental health system professionals, young people and their families) raised eating disorders as a top priority (Cambridgeshire and Peterborough Integrated Care System, 2022a).
Policy context
Eating disorders were raised by local stakeholders (mental health system professionals, young people and their families) as a key priority in the local Children and Young People’s Mental Health Strategy in 2022 (Cambridgeshire and Peterborough Integrated Care System, 2022a). The strategy committed to achieving the following goals by 2025 (Cambridgeshire and Peterborough Integrated Care System, 2022c):
- Meet the rising demand for help with disordered eating (success will be measured by a year-on-year increase in help and treatment for disordered eating).
- Ensure there is specific help and treatment across the spectrum of need for disordered eating.
- Ensure touch points with families (such as education and faith communities) are equipped with the basic skills and information to recognise and respond appropriately to disordered eating.
- Commission or support coproduction projects around the needs of children and young people with disordered eating.
- Provide positive and constructive information to young people about disordered eating, that challenges stigma and promotes getting help.
Other recent strategies have also made commitments to improving eating disorder support:
- The NHS Long Term Plan (2019) committed to boosting investment in children and young people’s eating disorder services, in order to maintain the goal of seeing 95% of urgent cases within 1 week, and within 4 weeks for non-urgent cases (NHS, 2019).
- The local Children and Young People’s LTP (2021) committed to developing a core service, home treatment, a commissioned medical monitoring pathways (linking between specialist services and primary care) and support for people with avoidance restrictive food intake disorder (ARFID) (Cambridgeshire and Peterborough Clinical Commissioning Group, 2021).
- The Cambridgeshire and Peterborough All-age Autism Strategy (2021) highlighted that need for appropriate mental health information for neurodiverse children and young people, and their families, including information around disordered eating (Cambridgeshire County Council & Peterborough City Council, 2021).
- Eating disorder services in Cambridgeshire and Peterborough have recently undergone transformation in key areas, including the development of home treatment offers and a medical monitoring pathway with a clear link between specialist services and primary care. This transformation was delayed by the COVID-19 pandemic.
Mental health need
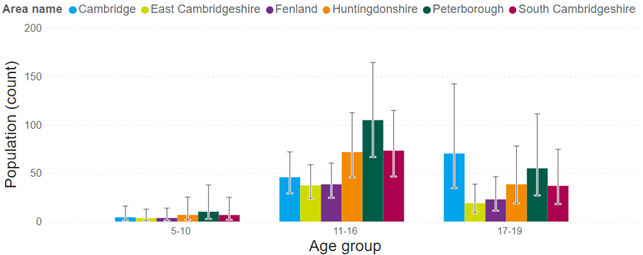
It is estimated that there are 649 children and young people under age 20 with an eating disorder in Cambridgeshire and Peterborough (95% confidence interval: 365 – 1,205). This definition was based on disturbances in eating behaviours, appetite or food intake; and includes anorexia nervosa, bulimia nervosa, and binge-eating. 60% of children and young people estimated to have an eating disorder are aged between 11 and 16.
Figure 39: Estimated numbers of children and young people (aged 5 to 19) with eating disorders in Cambridgeshire and Peterborough, 2023. Data source: dashboard
There is anecdotal evidence from local professional that there has been a rise in the complexity of eating disorder presentations in recent years.
How common are eating problems?
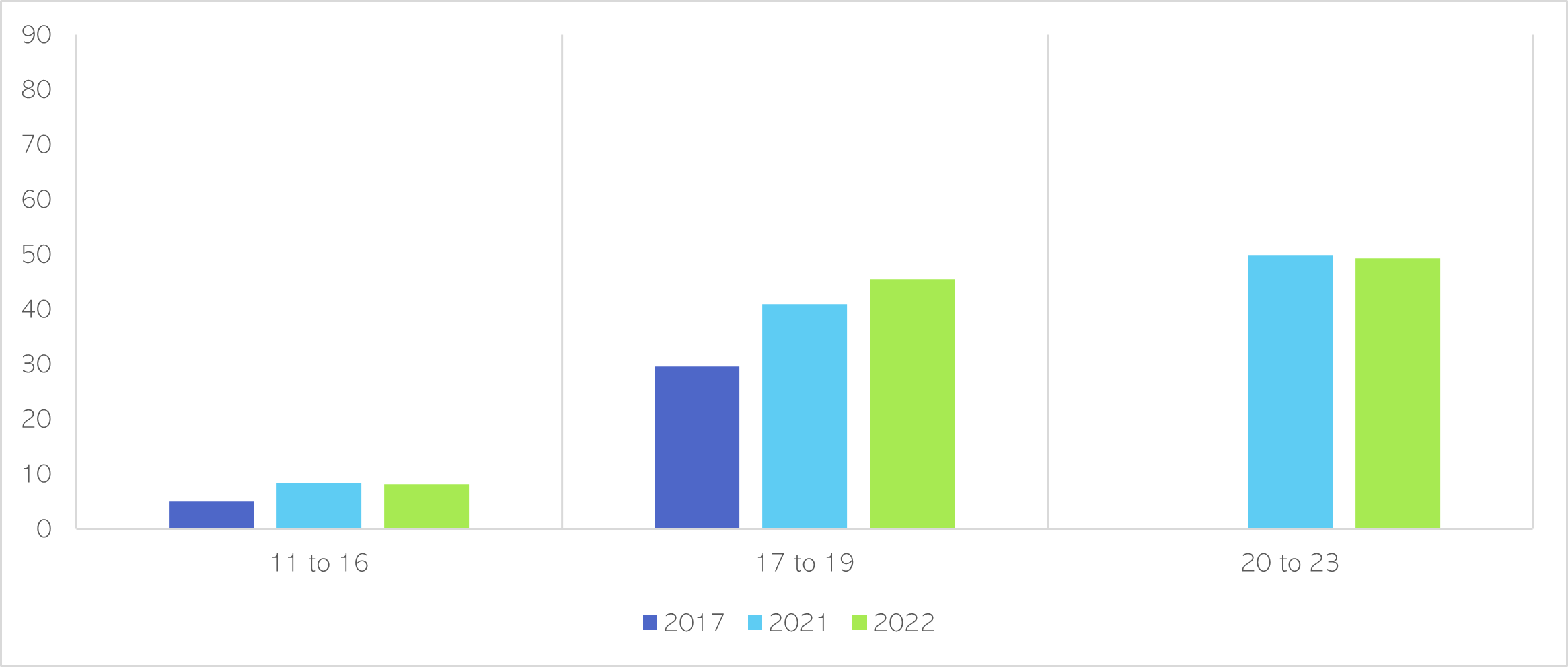
Nationally, an increasing number of young people aged 17 to 19 are screening positive for possible eating problems (NHS Digital, 2022). ‘Eating problems’ do not mean that the someone has an eating disorder but indicates an increased likelihood of problems with eating. For boys and young men, the greatest increase in eating problems over the past 5 years has been in the 17 to 19 age group (NHS Digital, 2022).
Figure 40: Proportion of boys and young men screening positive for possible eating problems by age, 2017, 2021 and 2022. Data source: (NHS Digital, 2022). Note that screening positive does not mean that the child or young person has an eating disorder but indicates an increased likelihood of problems with eating. Young people aged 20 to 23 were not asked this question in 2017.
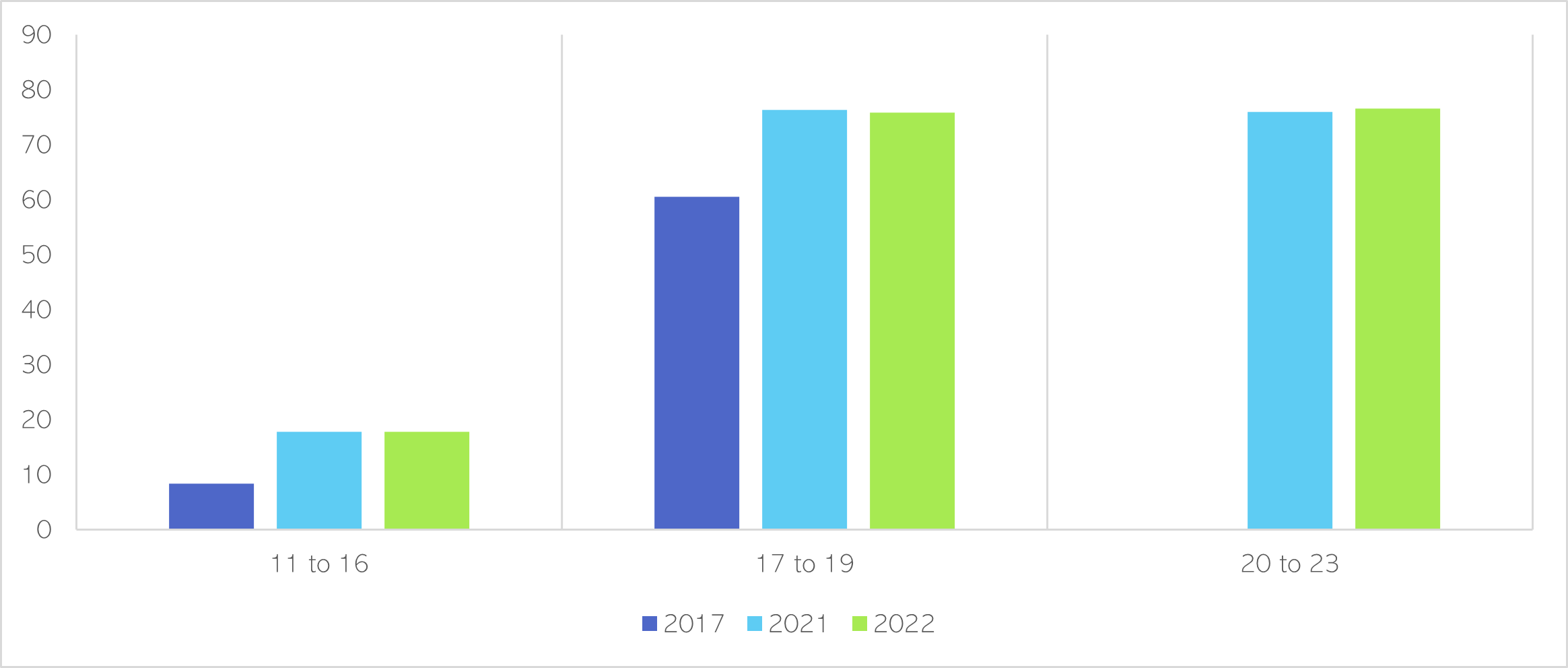
Since 2017, there has been a rise in the number of young women screening positive for possible eating problems. There was a large increase in 11- to 16-year-olds (from 8.4% to 17.8%), as well as in the 17 to 19 age group (from 60.5% to over 75%) (NHS Digital, 2022).
Figure 41: Proportion of girls and young women screening positive for possible eating problems by age, 2017, 2021 and 2022. Data source: (NHS Digital, 2022). Note that screening positive does not mean that the child or young person has an eating disorder but indicates an increased likelihood of problems with eating. Young people aged 20 to 23 were not asked this question in 2017.
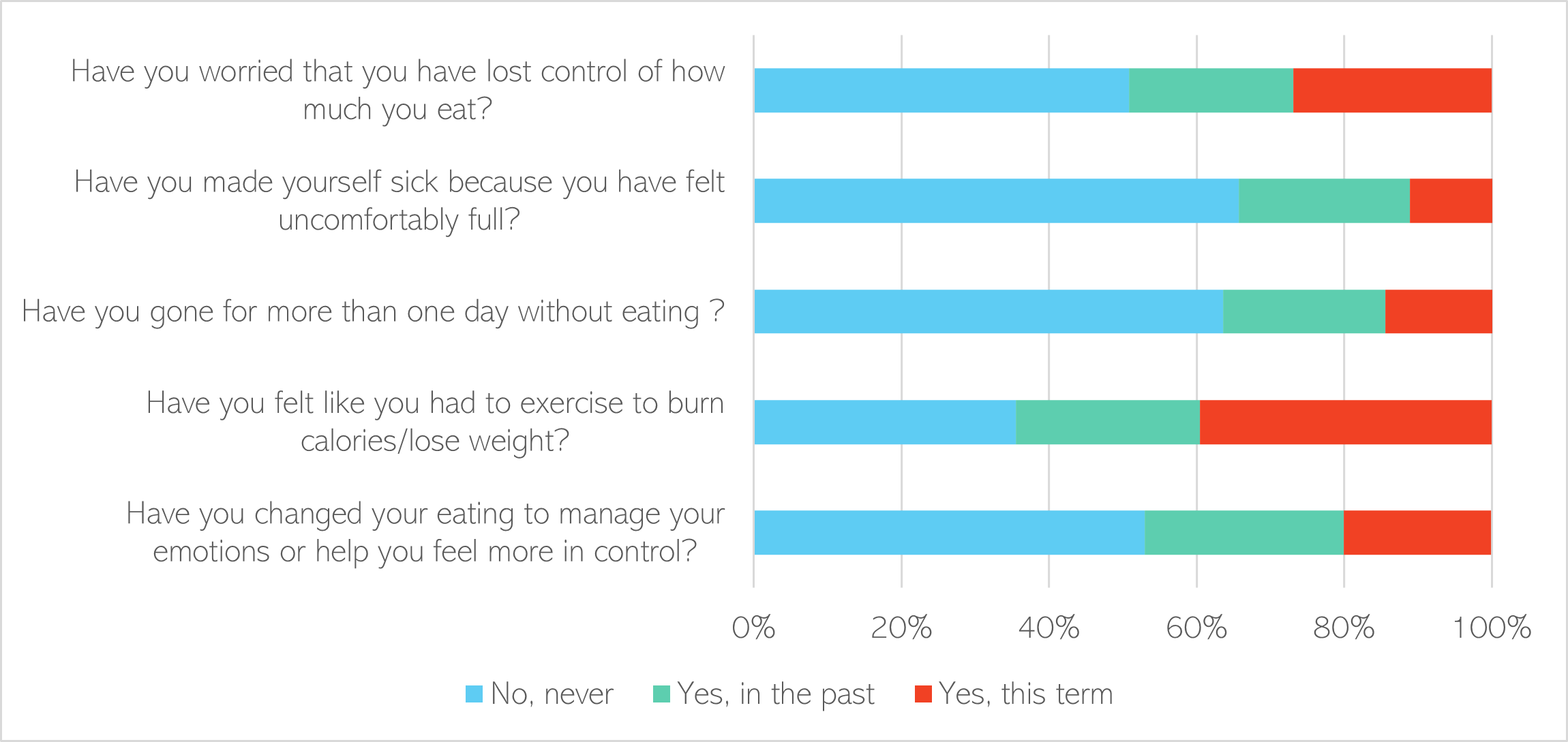
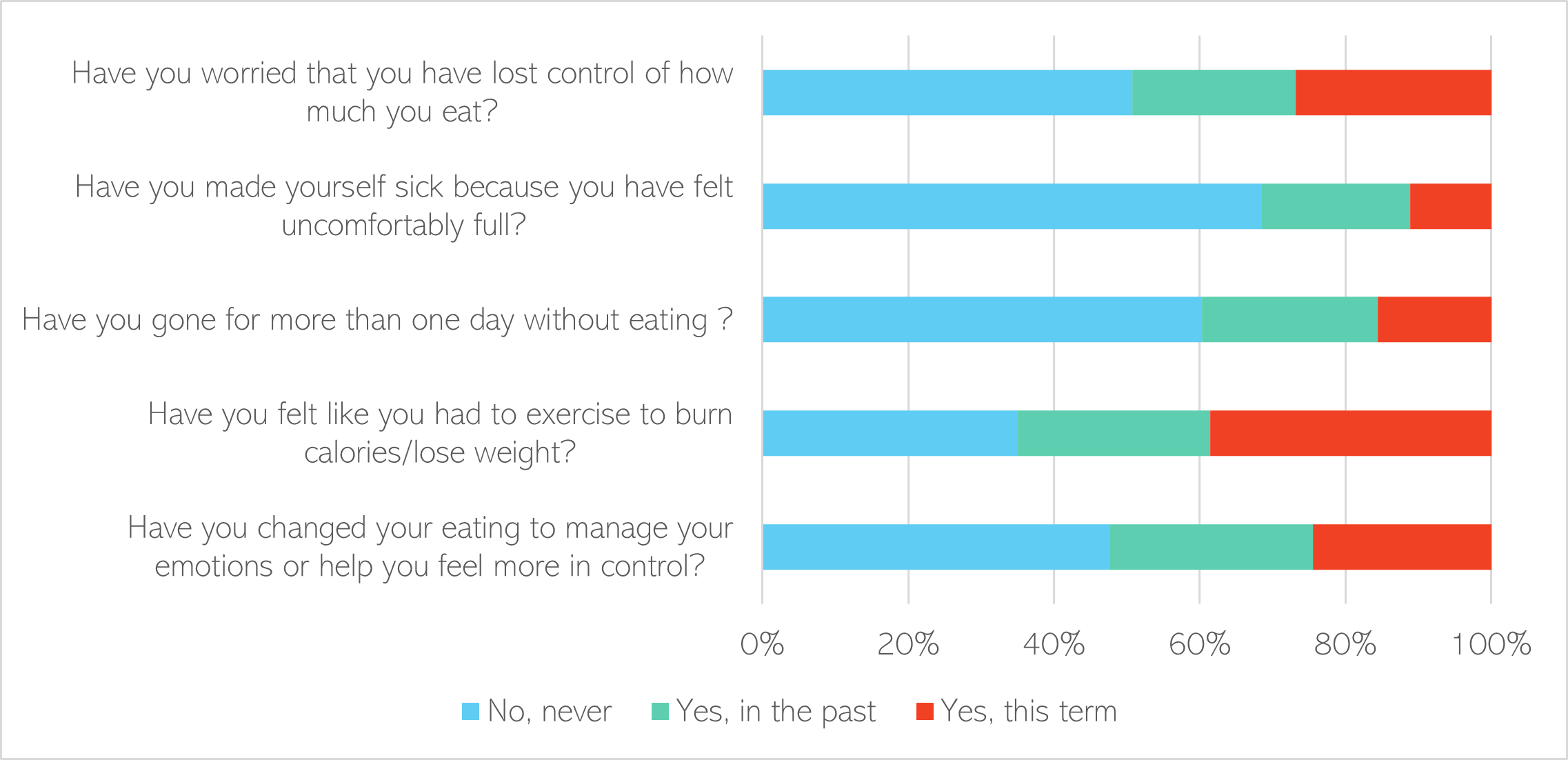
Local data from the 2022 health-related behaviour survey shows that a significant proportion of Year 8 pupils (aged 12 to 13) in Cambridgeshire and Peterborough had worries around food. A high proportion have felt they needed to exercise to burn calories or lose weight; and have been worried about losing control of how much they have eaten. 3.0% of Year 8s had ever used weight loss medication or laxatives to lose weight.
Figure 42: Self-reported eating behaviours of Year 8s in Cambridgeshire and Peterborough. Data source: Health-related behaviour survey 2022. Note: missing data, where students did not answer this question, was excluded from this graph.
There were similar eating behaviours in Year 10s (aged 14 to 15) in Cambridgeshire and Peterborough. 3.8% of this year group had ever used weight loss medication or laxatives to lose weight.
Figure 43: Self-reported eating behaviours of Year 10s in Cambridgeshire and Peterborough. Data source: Health-related behaviour survey 2022. Note: missing data, where students did not answer this question, was excluded from this graph.
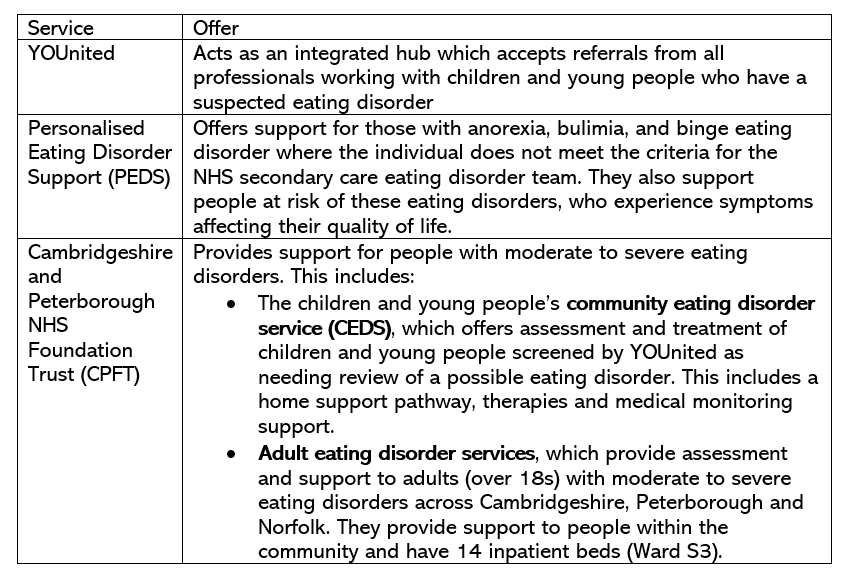
Service provision
Service use
The Children and Young People’s Mental Health Strategy included a review of local mental health services but did not focus on eating disorders services, which were grouped under the wider umbrella of ‘specialist mental health teams’ (Cambridgeshire and Peterborough Integrated Care System, 2022b).
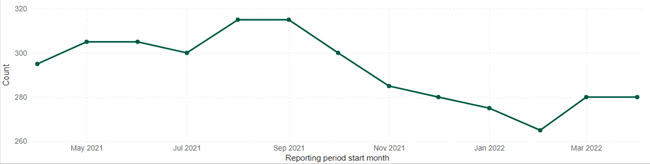
Over the past few years, new monthly referrals with eating disorder issues increased from September 2020. They were elevated throughout the early stages of COVID-19 pandemic and remained above baseline by Spring 2022.
Figure 44: New referrals with eating disorder issues. Data source: Mental Health Services Data Set
The waiting list for treatment for eating disorders in Cambridgeshire and Peterborough decreased at the start of 2022, from a peak of 315 in August and September 2021 to 280 in April 2021.
Figure 45: Referrals with eating disorder issues waiting for treatment at the end of each month, where patients are aged between 0 and 18. Data source: NHS Mental Health Services Dataset
References
Full list of references is included at the end of this chapter.